Laparoscopic Duodenal Switch
The bariatric duodenal switch surgery is also known as a biliopancreatic diversion with duodenal switch or DS. The procedure is a combination of restrictive and malabsorptive weight loss surgeries. The goal of this approach is to decrease the amount of food the stomach can accommodate and limit the length of intestine which absorbs calories, as well as reduce overall calorie intake.
If you’re interested in starting your weight loss journey with bariatric surgery, contact Dr. Lutfi for duodenal switch surgery in Chicago, IL.
What Makes Bariatric DS Surgery Different?
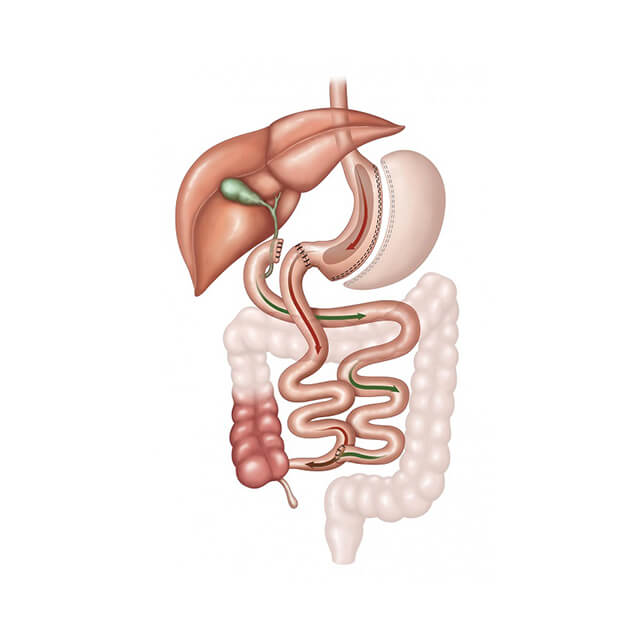
The biliopancreatic diversion with duodenal switch (BPD/DS) treatment has two components. The first is similar to the sleeve gastrectomy method. Dr. Lutfi creates a small, tubular pouch by removing part of the stomach. The second portion of treatment is bypassing much of the small intestine, which is part of traditional gastric bypass surgery.
The duodenal switch results in a moderately sized stomach pouch and the bypassing of a significant part of the small intestine. These outcomes allow the patient to lose weight without a substantial deviation from their eating habits, compared to what is required by other types of bariatric surgeries. After treatment, the stomach can hold about five to six ounces of food, while other procedures typically allow only a half to one full ounce.
To learn more about the laparoscopic duodenal switch, please contact our office to schedule a consultation and evaluation. Call (877) 396-8226 today.
The BPD/DS Bariatric Procedure with Dr. Lutfi
 The duodenal switch surgery begins with strategically placing several half-inch incisions in the middle of the abdomen. As laparoscopic surgery is minimally invasive, these are the only incisions necessary to perform the changes to both the stomach pouch and create a bypass. A thin tubular device called a laparoscope is placed at the treatment site, allowing Dr. Lutfi to perform the duodenal switch method.
The duodenal switch surgery begins with strategically placing several half-inch incisions in the middle of the abdomen. As laparoscopic surgery is minimally invasive, these are the only incisions necessary to perform the changes to both the stomach pouch and create a bypass. A thin tubular device called a laparoscope is placed at the treatment site, allowing Dr. Lutfi to perform the duodenal switch method.
The fiber optic video camera, along with special surgical instruments, helps Dr. Lutfi precisely perform the duodenal switch surgery. Because this technique involves small incisions, recovery times are shorter with less discomfort than with the traditional surgeries, where more invasive methods were required to create the same effect.
Dr. Lutfi creates a shortcut to the newly resized stomach pouch by rerouting the small intestine and connecting a portion that is lower on the track. This allows food to pass through the newly created pouch and into the last portion of the small intestine directly. Nearly three-quarters of the small intestine are bypassed, reducing overall food and caloric intake. All enzymes and required to break down fats and proteins for proper absorption enter the small intestine through the newly created shortcut. This allows these important components to mix freely with food intake for proper digestion.
How Does DS Surgery Promote Weight Loss?
This method affects how your body processes foods. As food does not mingle with the enzymes and until farther down the small intestine, there is a substantial decrease in the absorption of nutrients and calories (especially fats and proteins), as well as vitamins and nutrients needing fat for absorption (fat-soluble nutrients and vitamins).
The duodenal switch, like the sleeve gastrectomy and gastric bypass, affects gut hormones in a manner which impacts blood sugar control, satiety, and hunger. The BPD/DS is considered the most effective surgery compared with Adjustable Gastric Band (AGB), Sleeve Gastrectomy (LSG), and Gastric Bypass (RYGB).
The Advantages of Duodenal Switch Surgery
- Results in around 70% loss of excess weight loss after five years
- Allows patients to enjoy near-normal amounts of food eventually
- Decreases fat absorption
- Causes an improvement in satiety and a reduction in hunger by positively affecting hormone levels
- Is the more effective against diabetes when compared to AGB, LSG, and RYGB
What to Consider about your DS Procedure
- It is critical to comply with vitamin and dietary supplement guidelines, follow up visits, and aftercare to avoid the potential risks from vitamin and protein deficiencies.
- Duodenal switch treatment has a greater risk of long-term deficiencies of vitamin D, zinc, calcium, iron and other vitamins
- Higher risk than RYGB, LSG, and AGB
- Like all bariatric surgeries, treatment is not quick; the duodenal switch procedure is about combining the surgery with diet and exercise to optimize weight loss results.
Duodenal Switch Recovery
 After your procedure, you will be moved to a recovery room for observation. When Dr. Lutfi is satisfied with your progress, you will rest in the hospital for one to two nights. Here, you will be helped up by a nurse or practitioner to move and walk gently. This movement will promote blood circulation and healing.
After your procedure, you will be moved to a recovery room for observation. When Dr. Lutfi is satisfied with your progress, you will rest in the hospital for one to two nights. Here, you will be helped up by a nurse or practitioner to move and walk gently. This movement will promote blood circulation and healing.
You may require oxygen transiently and will be provided pain medication as needed, along with compression garments to prevent blood clots. You will be given liquids soon after surgery and soon realize you become satisfied with smaller meals.
Expect frequent visits from Dr. Lutfi and different staff on his team to monitor your progress and handle any complications which may arise. In routine cases, you will stay overnight, and no blood work or X-rays are needed. However, depending on your progress, you may stay longer, and blood work or X-ray may be needed.
Life After Duodenal Switch Surgery
The duodenal switch surgery delivers excellent results; patients lose around 70% of their excess weight in the five years following surgery. However, patients must compensate for nutritional losses caused by a shorter connection between the stomach and small intestine. The patient can take supplements, which include the vitamins and minerals needed for a healthy lifestyle. In almost all cases, these supplements are a lifetime requirement.
Long-term, most patients that choose duodenal switch surgery experience lasting results. Lifestyle changes are not as drastic as with other types of bariatric surgery. The duodenal switch patient also experienced increased satisfaction with treatment as they can eventually eat larger portions than those with restrictive surgeries.
The possibility of eating more than with other procedures while still losing weight is attractive to many candidates considering bariatric surgery. However, few surgeons perform a duodenal switch, so it is important to understand the challenges of travel for follow up visits. Dr. Lutfi and his staff can help arrange any special considerations to make the patient available for follow up visits.
To learn more about the laparoscopic duodenal switch, please contact our office to schedule a consultation and evaluation. Call (877) 396-8226 today.
Duodenal Switch FAQs
Because the duodenal switch combines malabsorption with moderate intake restriction, the patient sees a higher percentage of excess weight loss than with other procedures. According to the Obesity Surgery Magazine, Type II Diabetic patients see a cure rate as high as a 98% and sleep apnea patients as high as a 92% improvement. Post-surgery diet is also more enjoyable than what is required after other bariatric surgeries.
No. Because Duodenal switch surgery removes a large part of the stomach, it is not reversible.
Because of the higher risk with duodenal switch surgery than other weight loss procedures, patients must meet the high Body Mass Index (BMI) of 50 and have not been capable of losing weight with other methods.
High-risk health conditions like heart disease and liver disease may eliminate potential candidates from duodenal switch surgery.
The ASMBS (American Society for Metabolic and Bariatric Surgery) states duodenal switch surgery is a great solution for type II diabetes. Improvement rates are high, up to 95% improvement can be expected from this procedure.
The Bariatric Medical Institute claims that duodenal switch surgery has shown improvement in asthma, type II diabetes, sleep apnea, anxiety, depression, and heart disease.
Potential risks include:
- Vitamin or mineral deficiencies
- Pouch clogging
- Bleeding
- A hernia
- Ulcers
- Blood clots
- Leaks
Because duodenal switch surgery helps obesity-related issues like diabetes and heart disease, most insurance providers will help with the costs to avoid other obesity-related health conditions.
Dr. Lutfi often orders the following tests before duodenal switch surgery (in addition to others, depending on the unique patient case):
- Upper endoscopy
- Medical evaluation
- Depending on your health, cardiology or pulmonary evaluation may be required
- Dietary evaluation and education
- Psychological evaluation (most patients chose to continue with the psychological visits after surgery to support their positive changes)
- Blood work and EKG
You will be limited to a liquid diet or pureed foods during the first month following surgery. When you can tolerate these foods without nausea, soft foods can be added to your diet with solid foods later. Chewing all foods is important, and beverages should not be consumed during meals.
You should eat 90 grams of protein daily so your digestive tract can deliver proper nutrition to your body.
Due to limited absorption, it is recommended for all patients to take extra vitamins, such as multivitamin, vitamin B12, calcium and iron. Our full-time dietitian and nurse will give details of the dosing and types of supplements. We will check your vitamin levels periodically to ensure good health. This is one of the reasons for the mandatory follow-ups with our team.
You should walk as often as possible but not to the level of discomfort. You should avoid strenuous activity for at least a month. After a month, you should walk at least a half hour every day.
The American Society for Metabolic and Bariatric Surgery warns that some hair loss is possible. This loss is a result of nutritional changes and stress. The problem is often temporary, and hair loss will stop after the initial rapid weight loss period at about six months to one year.
You may shower as soon as you feel up to it, but keep your incisions dry. Do not bathe or submerge yourself with water for two weeks.
You can drive as soon as you are off your pain medications.








